You’re digging through end-of-month reports to find out which payers aren’t paying.
business of diagnostics
Technology
Revenue
Revenue Cycle Assessment
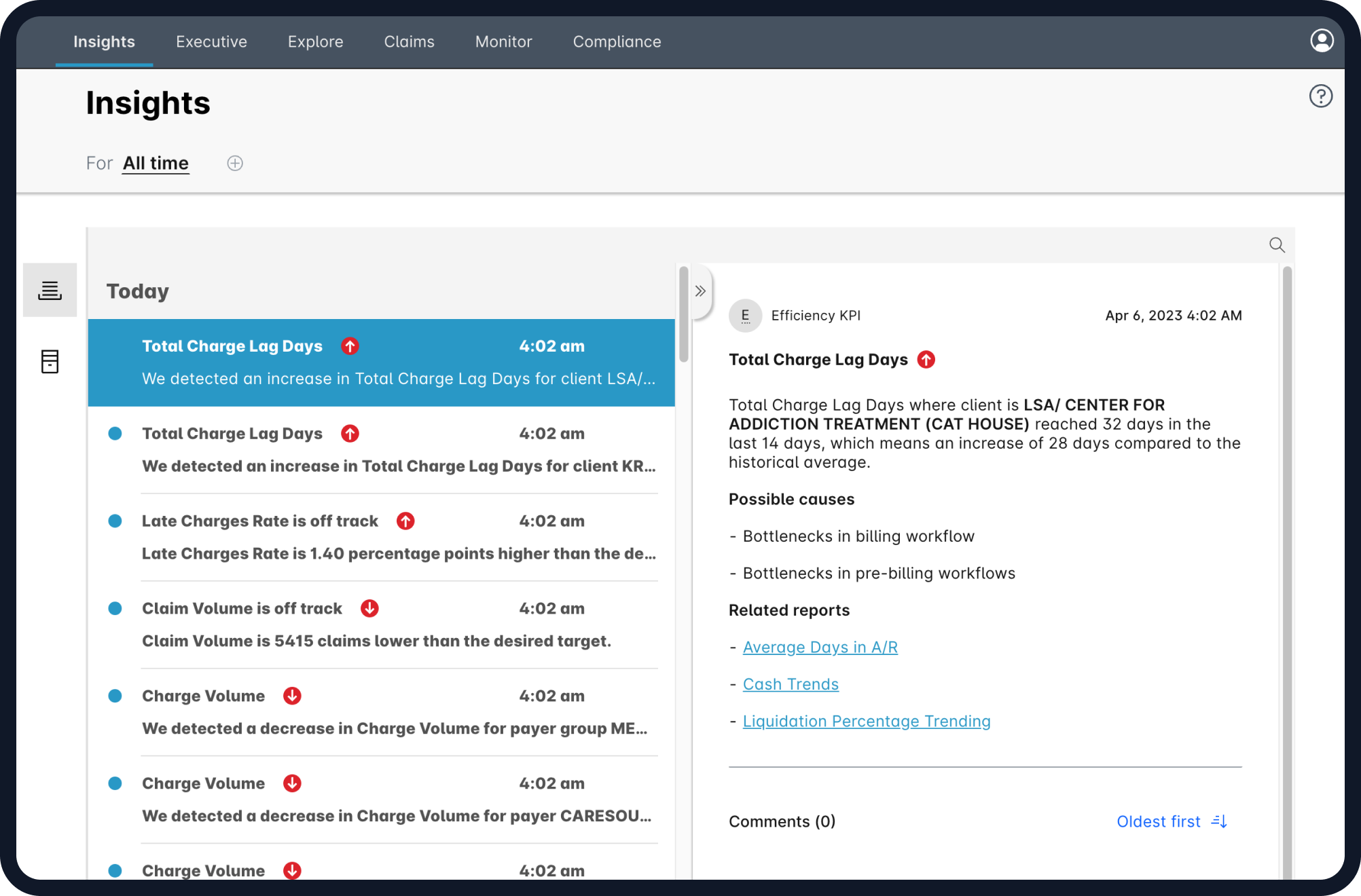
Identify, and prevent issues that lead to decreased revenue performance
Revenue Monitoring
Predictive Adjudication & Payer Reimbursement Monitoring
Commercial Analytics
Commercial Analytics to Drive Profitable Golume Growth
Underpayment Detection
Underpayment Detection of Claims for On-Time Appeals
Resources
-
Revenue Cycle Assessment Identify, and prevent issues that lead to decreased revenue performanceRevenue Monitoring Predictive Adjudication & Payer Reimbursement MonitoringCommercial Analytics Commercial Analytics to Drive Profitable Golume GrowthUnderpayment Detection Underpayment Detection of Claims for On-Time Appeals